Psilocybin and Depression; Psychedelics Can Reset Brain Function

Psychotropic plants once considered taboo are now being used as highly effective clinical solutions for treating a number of psychological issues, including depression, PTSD, and end-of-life anxiety.
And recent studies have gained traction using psilocybin, the psychoactive compound in ‘magic’ mushrooms, as a successful treatment for depression. The study found evidence of a reset mechanism in the brain triggered by psilocybin that can have lasting effects.
Psilocybin & Depression
A calm, relaxed feeling in the hours, days, and weeks after using psilocybin is familiar to those who have taken it before. This is sometimes referred to as an “after-glow,” and many attribute this to the sense of profundity or universal insight acquired during the experience. This sensation is often subjective and fleeting – something that would be difficult to measure in a lab.
But now a team of researchers has set out to measure this feeling and the potential it has for use as a clinical treatment for depression and anxiety. These researchers believe they have possibly recorded this reaction and noticed a reconfiguration of the neural pathways in patients, which they say have become narrowly reinforced in people experiencing severe depression and anxiety. Their research appears to show what they call a disintegration and reintegration in which psilocybin acts as a “reset mechanism.”
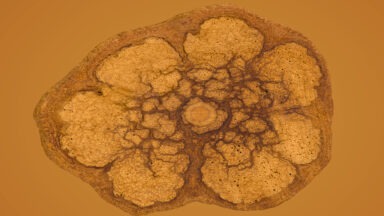
This test, conducted by researchers at Imperial College London, looked not only at subjective measures of how patients felt in the days and weeks after receiving a dose of psilocybin but also more objective measures seen in brain scans that monitor cerebral blood flow and functional connectivity. The scientists focused on the amygdala, an area of the brain where emotion, behavior, and motivation are processed, noticing that decreased cerebral blood flow to this particular location correlated with reduced depressive symptoms.
The amygdala is directly connected to the prefrontal cortex, controlling a sort of back and forth process for measuring fear. This is basically where your fight or flight response plays out. The amygdala acts as our alarm system, sending a signal to the prefrontal cortex, which in turn tells it whether that threat is something to actually be concerned about. It’s thought that higher activity in the amygdala leads to lower activity in the prefrontal cortex which causes anxiety and depression.
This has led scientists to see psilocybin as an appropriate medicine for people experiencing anxiety and depression. But psilocybin isn’t the only psychedelic shown to have this effect. And while these material observations seem to correlate things like blood flow and electrical activity with those positive changes, some still maintain that the mystical psychedelic experience rather than the plant is what is so palliative.
Enter your email below to receive a free ebook
A Guide To Various Plant Medicines and Their Therapeutic Benefits
LSD for Depression
Similar studies have been undertaken with LSD in place of psilocybin, providing similar results. The most well-known trials have been conducted by MAPS, the Multi-Disciplinary Association for Psychedelic Studies, a group that has been working on advancing clinical research with psychedelic and empathic drugs for the treatment of depression, anxiety, and PTSD.
A 2014 study administered LSD to 12 patients experiencing severe depression, anxiety, and end-of-life anxiety, 11 of whom had never taken the drug before. Nearly all who completed the trials expressed the desire to receive more treatments in the future due to their notably positive experiences.
One subject said the experience caused a marked shift in her values to make time for things that were more important in life, like family. Another subject with end-of-life anxiety found that after her LSD experience she found humor in her illness and looked at herself as part of a larger cosmic entity rather than an individual. Meanwhile, all subjects reported no lasting adverse side effects after the experience.
While these clinical studies show promise and work well in closely monitored environments accompanied by professional psychotherapy sessions, many remain unconvinced due to the smaller data set of studies and subjects. But this is primarily due to strict laws preventing these trials as well as difficulty obtaining compounds from legitimate sources.
However, a recent shift in the public perception regarding psychedelics and cannabis seems to be bucking the trend. Meanwhile, groups like MAPS and the Beckley Foundation are helping ease the stigma, stating their belief that more psychedelic compounds will be approved for clinical use in coming years.
Ketamine Depression Treatment
Clinical trials for treating depression with LSD and psilocybin often lead critics and journalists to harken back to the ’60s and make some clichéd quip about the hippie generation, or their brief stint experimenting with drugs in college. But when it comes to ketamine, personal anecdotes are fewer and far between. This drug, which tends to also fall into the recreational club-drug scene, has shown some profound results when it comes to its potential for treating severe depression, especially for those who are suicidal.
Though ketamine for treating depression is considered an off-label drug, one that is used for a purpose other than what it is labeled for, it has shown unprecedented results. Typically used as an anesthetic, in large doses ketamine is a highly psychoactive hallucinogen, and also an antidepressant.
People who are suicidal and have not had success with typical antidepressants have seen drastic changes within a few hours of ketamine treatment. Researchers believe that ketamine acts on glutamate, rather than serotonin and dopamine, the chemicals most antidepressants focus on. This particular channel can cause drastic changes and overnight transformation in attitudes of people suffering from severe depression.
Of course, doses high enough to achieve this effect are incapacitating and can be difficult to deal with. The psychedelic effect of ketamine can lead to “k-holes” or feelings of intense and sometimes frightening psychedelic experiences often paired with paralysis. This has lead doctors to search for drugs that can target the glutamate in the brain, but skip a burdensome trip.
While these drugs have amazing potential to help solve mental issues that plague large percentages of society, there needs to be a shift in drug policy to allow them to be rescheduled. Almost all of these drugs are Schedule 1, classified as having no medical value, but clearly, there is plenty of evidence to the contrary.
While their use should be monitored and administered in a controlled set and setting, their criminalization prevents people from taking advantage of the positive results scientists are seeing. And when an effective drug is made illegal, it can lead to those who need it seeking it out on the street where purity and quality aren’t guaranteed.
Study Shows Microdosing Psilocybin Boosts Mood, Mental Health

A new study provides the most compelling evidence to date on the impressive mental health benefits of microdosing psilocybin.
While there has been an ever-increasing number of studies showing the efficacy of treatment of mental health disorders with psychedelics, there has been relatively little research on the practice of microdosing.
Microdosing, or repeatedly taking small, barely perceptible amounts of psychedelics, has been exponentially increasing in popularity, with a wide range of people reporting a multitude of improvements to their psychological wellbeing.
The latest scientific study to look at the effects of microdosing was conducted by researchers at the University of British Columbia, as well as other leaders in the fields of psychology and mycology. The study followed 953 people who used small, repeated doses of psilocybin for about 30 days, as well as a control group who did not microdose.
While the exact dosages of psylocibin that participants self-administered varied somewhat, they were all low enough to not impact daily functioning.
Over a one-month period, participants took these psylocibin microdoses three to five times per week and were asked to complete a number of assessments through a smartphone app that tracked their mental health symptoms, mood, and measures of cognition. The findings definitively showed that the microdosing participants demonstrated greater improvements in mood and mental health than those in the non-microdosing control group.