Guide to Alternative Medicine Part 1: Traditional Chinese Medicine
“When health is absent Wisdom cannot reveal itself, Art cannot become manifest, Strength cannot be exerted, Wealth is useless and Reason is powerless.”
— Herophilies, 300 B.C.
Just a decade ago, if patients wanted to explore unconventional treatment options they were on their own. Traditional health professionals generally didn’t encourage alternative therapies or treatments, and discouraged departures from allopathic treatment models such as drugs and surgery.
As research validates the efficacy of non-traditional treatment models, such as traditional Chinese medicine (TCM), ayurvedic medicine, massage and chiropractic adjustment, naturopathy, diet, and natural supplementation — even homeopathy and sound therapy — new branches of medicine emerge.
Integrative, Functional, Complementary, and Alternative Medicine
The “integrative” medical model developed during the early 1990s but was formalized when the National Institute of Health (NIH) created the National Center for Complementary and Integrative Health (NCCIH). This classification covered non-conventional treatment and research, and was the beginning of a slow recognition of alternative systems. Integrative models include consideration of a patient’s lifestyle, body, and mind, and how to promote well-being for the whole person rather than just diseases and their symptoms.
“Functional” medicine refers to holistic and alternative medical practices intended to improve overall functions of the body’s systems and explores individual biochemistry, genetics, and environment to determine underlying causes of disease.
According to the NIH, “complementary” medicine coordinates non-mainstream practices with conventional treatments. This has driven acceptance of alternative therapies such as TCM, diet, and nutraceuticals, or supplements.
Alternative medicine is any practice that falls outside conventional systems and is not combined with traditional treatments. For example, if patients choose Ayurvedic medicine, dietary changes, and supplementation to treat their cancer and exclude conventional therapies, they have entered the realm of alternative medicine.
Traditional Chinese Medicine
“Those who disobey the laws of Heaven and Earth have a lifetime of calamities while those who follow the laws remain free from dangerous illness.”
— Huangdi, The Yellow Emperor, 2698–2598 BCE
Traditional Chinese Medicine (TCM) claims to be the third-oldest medical system, preceded only by Egyptian and Babylonian medicine. Theories of TCM are believed to be at least 3,000 to 4,000 years old — likely older, predating written language.
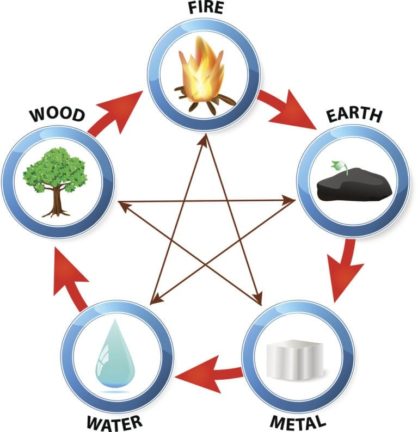
The foundations of TCM are meridian channels and acupuncture points that conduct the movement of chi, and the five-element model correspondences to these points and channels. This five-element system of wood, fire, earth, metal, and water also applies to seasons, colors, sounds, sense organs, personality types, Chinese astrology, feng shui, the I Ching, and countless other aspects of Chinese culture and life.
The Five-Element System in Chinese Medicine
Called the Wu Xing, this five-element system defines relationships between the elements and considers them to be in continual active cycles wherever they are found. Mother/child, or generating relationships, are: wood fuels fire, fire forms earth (think of volcanic flow and ash) earth produces metal, metal carries water (buckets, pipes, etc.), and water feeds wood.
Conversely, there are antagonistic (father/child) relationships: fire melts metal, metal penetrates wood (ax, saw), wood separates earth (tree roots break soil), earth absorbs and directs water (river banks), and water extinguishes fire.
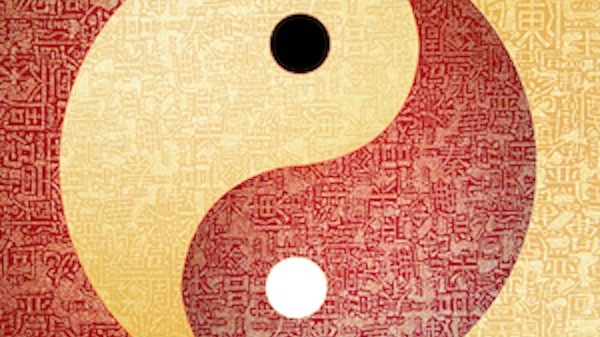
Chinese and Taoist doctors, called OMDs (oriental medicine doctors), see a patient through this lens of five-element relationships, along with yin and yang (passive and active) qualities. Organs are paired into male and female element families that include seasons, colors, compass directions, sense organs, emotions, and virtues. The female, or yin, organs are continually active — the Chinese say a woman’s work is never done — while male yang organs have periods of rest and activity. Element family qualities are:
-
- Metal: Lung (yin), large intestine (yang); season: autumn; color: white; direction: west; sense organ: nose; emotion: grief. When balanced, grief becomes the virtue of integrity.
- Water: Kidneys (yin), bladder (yang); season: winter; color: black; direction: north; sense organ: ears; emotion: fear. When balanced, fear becomes the virtues of poise, calm, and alert stillness.
- Wood: Liver (yin), gall bladder (yang); season: spring; color: green; direction: east; sense organs: eyes; emotion: anger. When balanced, anger becomes the virtue of kindness.
- Fire: Heart (yin), small intestine (yang); season: summer; color: red; direction: south; sense organ: tongue; emotion: rush/rudeness. When balanced, rushed rudeness becomes the virtues altruism and joy.
- Earth: Spleen (yin), stomach(yang); season: late summer; color: yellow; direction: center or middle; sense organ: mouth; emotion: worry and overthinking. When balanced, worry and obsession become the virtues of balance and equanimity.
The five-element paradigm is so pervasive that when someone is having a temper tantrum, the Chinese assume the fit is related to a liver imbalance. By using internal yogas, an organ’s emotion can be “cooled,” or transmuted, to its virtue. As the saying goes, “If angry, do the liver-calming exercise eight times. If you’re still mad, the person who angered you deserves to be slapped.”
The Taoists believe the organs have their own awareness and identities — happy organs make good health. They visualize each organ’s associated element color within the organ while acknowledging and thanking it for its service.
Traditional Chinese Medicine
Diagnostic Systems in TCM
In Chinese medicine, diagnosis is viewed as an art form. From the TCM perspective, imbalances in the yin and yang of the “functional entities” are the source of all illness. Disease may be caused by disturbances within an organ or disharmony between organs.
The functional entities are:
- The five fundamental substances: Shen (spirit), Jing (essence), Jinye (the body’s fluids except for blood), Xue (blood), and Qi or Chi, the body’s energy.
- Zang Fu: the Wu Xing, or five-element cycles of the five zang, or yin organs, and the six fu, or yang organs. The sixth yang organ is the triple warmer, considered a “radiant circuit” and a meridian, responsible for the body’s heat and energy.
- The Jing-luo, or channels and meridians, used for the body’s flow of chi.
TCM diagnostic methods include:
- Inspection of the face, skin, particularly the tongue.
- Odor, which corresponds to sound — called “auscultation.”
- Palpation, specifically wrist pulses and meridian points.
- Inquiry into a patient’s lifestyle, health, diet, and sleep.
Six Major TCM Treatment Methods
After diagnosis is made, an OMD has several treatment choices, and may prescribe one, a few, or all. Treatment methods include:
- Acupuncture: This is the TCM method most familiar in the west. An acupuncturist may or may not be an OMD, but an OMD always practices acupuncture. Using fine, sterile needles that have nothing in common with syringe needles used in conventional medicine, the practitioner targets specific points that can be located anywhere on the body, including in the ears, on toes and fingers, or the face. The acupuncturist’s goal is to move stagnant chi, calm overactive chi, rebalance the body’s elements, treat specific conditions such as inflammation, and promote wellbeing.Patients report acupuncture needle insertion is generally painless, and the needles feel nothing like a syringe injection. Hollow injection needles are much larger than the fine acupuncture needles; eight acupuncture needles can fit in one standard syringe needle. Often patients are unaware of precisely where the needles are placed. Common sensations include a slight tingling at the placement site, or sometimes a mild ache as blocked energy begins to move. Because disposable needles are sterile, chances of infection are near null.
A practitioner may prescribe multiple acupuncture sessions or complete treatment in one. Clinical studies, as cited by the University of California Center for Integrative Medicine, have shown acupuncture has effectively treated allergies, neck, back, post-operative, knee, and labor pain, morning sickness and nausea, hypertension, tennis elbow, PMS, depression, sciatica — even stroke.
There are other conditions that show less clinical evidence of treatment success, but as research continues, the list of treatable conditions, according to Western evidence-based medical models, will likely grow. Migraine sufferers, those with substance addiction, arthritis patients, and many others have reported relief with acupuncture treatment. It should be noted that vast areas of TCM have not been subject to clinical research, though this in not an indication of whether or not the system is effective. It simply means Western research has not caught up with ancient, tried-and-true Chinese methods.
When choosing an acupuncturist, confirm the practitioner is properly licensed. While some chiropractors, physical therapists, or naturopaths may use needles for treatment, only a licensed acupuncturist will have comprehensive knowledge and training. If you see or feel a treatment space is less than clean, find another acupuncturist or OMD.
- Moxibustion: Called “moxa,” this heat treatment focuses over specific points with a burning stick of dried mugwort. The heat is therapeutic, and the patient is not burned, although in some rare instances, a practitioner will burn a specific point. Generally though, the sensation of moxa is soothing and comfortable. Moxa is also used to warm acupuncture needles in the skin. One technique is to place a piece of a sliced vegetable, such as potato or radish, on specific points, place the moxa herb on the slice, and light the moxa, allowing it to it burn until the moxa is ash.Moxa was and is practiced throughout Eastern and Central Asia — in Japan, China, Vietnam, Tibet, Korea, and Mongolia. Scientific research and findings on moxa are available at the National Center for Biotechnology (NCBI) Library of Medicine website.
- Herbology: Vast and complex, the TCM herbal system utilizes an estimated 6,000 plant, animal, fungi, and mineral substances. With 2,000-plus years of research, Chinese herbal knowledge dwarfs Western plant lore.Prescribed herbs are combined into tea or mixed with honey. Herbalists are now making tablets and capsules instead, as the honey pills are famously bad-tasting and hard to handle. Herbs are usually ingested several times a day, and practitioners may change herbal formulas several times over the course of a treatment.Herbalists make tonics by distilling and combining herbs and other substances. Tonics concentrate and intensify the herbs’ qualities and potency, and tonics are categorized as the most sophisticated use of herbs. Tonics are usually used to increase strength and vitality.
-
- Cupping: First-time visitors to an OMD or TCM practitioner may be surprised to find themselves face down on a table with small glass cups suctioned to their skin. Cupping, a.k.a. “Fire Jar Qi,” is used to dispel stagnant blood and lymph to relieve respiratory infections such colds, flu, pneumonia, and bronchitis.The suction action is created by heating the inside of the cup, then quickly placing it on the skin. A natural vacuum effect is created, and the cups are left in place until they fall off. Cupping leaves round, red marks on the skin that fade over time. This method is often used in combination with acupuncture.
-
- Tui Na Massage — Tui Na translates to “push and pull” in English. This designation covers many massage techniques used in TCM. an Asian form of massage, Tui Na has been practiced for centuries. This massage method employs acupressure, herbal ointments, compresses, and heat, and is most often used for musculoskeletal pain. Tui Na may be used as a stand-alone treatment, or integrated into a larger treatment plan to correct a patient’s disharmonies. This modality is often used on the elderly and infants, and is standard treatment in trauma, rehabilitation, and sports medicine in China.
- Taoist Medicine and Medical QiGong: Sometime before the 4th and 3rd centuries BCE, the Taoist system emerged as a religion, but historians are unable to agree on a true beginning date for the Tao, or for its most important text, the Tao Te Ching by Lao Tzu. No one knows when Lao Tzu lived, but the oldest known version of his text dates to the 4th century BCE.Taoist traditions are notoriously secretive. Their mysteries were compounded by the communist revolution purges of Taoist monasteries in the 1940s. Temples were destroyed, monks sent to labor camps, and survivors vanished into the mountains of China. Many feared the world had lost thousands of years-worth of accumulated Taoist wisdom and practices, but somehow, the traditions have survived, including the intricacies of Taoist medicine.
Taoist medicine principles expound the “Three Origins;” defined as “jing,” (essence), “Qi,” (a.k.a. chi, or energy), and “Shen,” (spirit), which are bestowed at conception. The system is rooted in a major Taoist theme, the unification of heaven, earth, and human. When our jing essence, stored in the kidneys, is exhausted, natural death occurs. It is possible to increase jing by going to sleep with unused chi, which converts to jing.
Intense adrenaline rushes and stimulant drugs such as cocaine directly deplete our jing reserve. Almost all stress reduces jing. According to Taoist teachings, jing herb tonics and advanced meditation practices protect the body from jing depletion.Immortality is a common goal for committed Taoists, and Chinese monks, priests, sages, and alchemists have worked for millenia to discover internal and external alchemical processes, longevity practices, meditations, and tonics to reverse the life cycle. This is reflected in Chinese iconography with the portrayal of the peach as a symbol for immortality, as well as the tortoise and the bottle gourd.The belief is that if a human achieves immortality, he or she will have the years needed to reach enlightenment, but achieving immortality alone may result in complete realization.Li Ching-Yuen, the oldest recorded Taoist practitioner, was an herbalist and martial artist who claimed to be 256 years old. Li Ching-Yuen observed Taoist meditation, breathing exercises, martial arts, and dietary practices, dying in 1933, as reported in the New York Times.

Taoist Medical Qigong
This is a category with its own specialized practitioners. It also functions as a stand-alone treatment system. Medical qigong does away with herbs, needles, and tools, instead relying on the practitioner’s use of his own chi to restore health and wellbeing. Called the most “ancient and sophisticated” form of treatment by Subhuti Dharmananda, Ph.D., the director of the Institute for Traditional Medicine.
Medical qigong requires years of training with a master practitioner. The methods derive from the esoteric branch of TCM, Taoist medicine, which includes internal energy practices, longevity yogas, herbology, talismans, incantations, and alchemy.
In the simplest terms, without touching the patient, the practitioner connects his own chi to the patient’s, consciously bringing the patient’s chi to equilibrium. The practitioner may also prescribe specific movements, such as those found in tai chi, to support treatment.
Although Western researchers have not confirmed the efficacy of medical qigong, it is a widely accepted treatment under the umbrella of TCM. Considered a preventative as well as a curative method, medical qigong is used to treat conditions including hypertension, cancer, depression, anxiety, addiction, or trauma, as well as degenerative disk disease, chronic pain, and diabetes.
Four Questions to Ask when Choosing an Acupuncturist or OMD
-
What are the Practitioner’s Qualifications?
There are multiple certifications for acupuncturists. The first requires a master’s degree from an accredited school of oriental medicine, usually a three- to five-year program. After earning a degree and passing written and practical exams, a practitioner earns an L.Ac., a license in acupuncture.
Another route is a certification from the National Commission for the Certification of Acupuncturists (NCCA). This requires a degree in oriental medicine from an accredited school or confirmation of a four-year apprenticeship. Qualifications are shown as Dipl. Ac. (Diplomate of Acupuncture) or Dipl. O.M. (Diplomate of Oriental Medicine). Also, ask if the practitioner is a doctor of oriental medicine (OMD)?
A medical doctor or osteopath may have L.Ac. as part of his or her title. This indicates completion of 100 to 200 hours of training in medical acupuncture.
It is completely acceptable to ask a practitioner about training and qualifications. If a practitioner is defensive when asked for information, move on.
-
Ask for Referrals
Check with your M.D. or primary healthcare practitioner as to whether he or she has preferred practitioners. Also ask friends and co-workers if they have experience with an acupuncturist, and if so, who they would recommend.
-
Ask if a Practitioner has Treatment Experience with Your Concern
It’s simple enough to call acupuncturists and request information as to whether they have treated a specific condition and how often.
-
Ask Whether the Practitioner has Malpractice Insurance
Malpractice insurance is confirmation that a practitioner has been through a complete review by an insurance provider, and qualifies for malpractice coverage.
Recent Acupuncture Research
- A recent study (December 2017) compared results of drug treatment vs. acupuncture for Alzheimer’s patients. The study concluded “acupuncture is safe, well tolerated, and effective in improving cognitive function” in patients with mild to moderate Alzheimer’s disease. Learn more here.
- An October 2012 study published in JAMA found acupuncture is an effective pain treatment for patients with chronic back and neck pain, osteoarthritis, headache, and shoulder pain, and indicated acupuncture is far more effective than a placebo.
- Breast cancer patients receiving chemotherapy drugs suffered fewer side effects, such as hot flashes, joint and muscle pain, and depression, when given acupuncture as an adjunctive therapy. This October 2013 study at the University of Maryland Medical Center, published in the American Cancer Society Journal, concluded that, for cancer therapy side effects, acupuncture is preferable to additional drugs as it produces no side effects of its own.
- Researchers at the Affiliated Hospital of Liaoning Traditional Chinese Medicine University found acupuncture, combined with an herbal paraffin treatment, was more effective in recovery and pain treatment for carpal tunnel syndrome. The study was published on the Healthcare Medicine Institute website in Jan. 2018.
Next: Alternative Health Care Part 2: Ayurvedic Medicine
The information in this article is intended for educational use only; it does not necessarily reflect the opinions of the Gaia Conscious Media Channel, and is not a substitute for professional medical advice, diagnosis, or treatment.
Introduction to Traditional Chinese Medicine
The Importance of Self-Care in Preventing Chronic Health Problems

Stress is part of life, but before it gets to be too much, it’s time to take care of yourself. Self-care is not selfish.
We all experience stress, it’s hardwired into our DNA; the fight or flight response is within each of us. But when we’ve been cooped up for too long, or events outside of your control way too heavily on your mind, it can all be too much. Mental stress can have serious negative effects on your physical health. That’s why it’s important to take care of yourself, especially if you take care of others or if you’re the type of empath that others lean on, you need to take a break.
To help others you must first help yourself.